Basal Cell Carcinoma
What is Basal Cell Carcinoma?
Basal cell carcinoma (BCC), is the most common skin cancer in New Zealanders.
It is estimated that around 40% of New Zealanders will develops a BCC during their lifetime. It is directly caused by exposure to ultraviolet (UV) light – even one severe sunburn in early life can lead to a BCC.
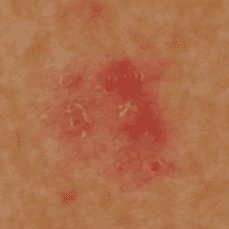
BCCs arise from the skin surface and generally grow very slowly over a number of months. It almost never spreads to other parts of the body. It can present in a number of ways ranging from a red scaly patch of skin, to a pearly lump with prominent blood vessels on the surface. Often a BCC can bleed easily with minimal trauma (eg when drying your skin with a towel). If left untreated the cancer will continue to grow and may cause ulceration of the skin and invade deeper structures.
There are a number of different ways to treat a BCC depending on the type of BCC and its location. Your specialist will discuss this with you if a BCC is diagnosed.
Get treated at the Skin Clinic
Published Literature
Growth of Periocular Basal Cell Carcinoma
E. Tan1*, F.P.Y. Lin2, L.H.N. Sheck3, P.J. Salmon1 and S.G.J. Ng3
1 Skin Cancer Institute, Dermatologic Surgery Unit, Tauranga, Bay of Plenty, New Zealand
2 Department of Medicine, Waikato Hospital, Hamilton, New Zealand and Centre for Health Informatics, University of New South Wales, Sydney, Australia
3 Department of Ophthalmology, Waikato Hospital, Hamilton, New Zealand
*Corresponding author
